Revolutionizing Medical Claims with AI-Powered Intelligence, Precision, and Speed
Unlock a new era of operational efficiency, financial accuracy, and patient satisfaction. Our advanced AI platform automates workflows, enhances compliance, and empowers faster decisions—so you can focus on what matters most: care.
The Pain Points
Medical Claims are Inefficient: Costly, Slow, and Prone to Error
Minimum Visibility
Insurers lack visibility into when and how much the next claims will cost
Massive Administrative Burden
Processing claims manually is time-consuming and resource-intensive
Costly Errors & Fraud
Manual review misses costly errors and fraudulent activities, leading to significant financial losses
Slow Reimbursements
Delays frustrate providers and patients, impacting cash flow and satisfaction. Processing can take weeks/months
Compliance & Audit Nightmares
Managing paper trails and ensuring compliance is complex and risky
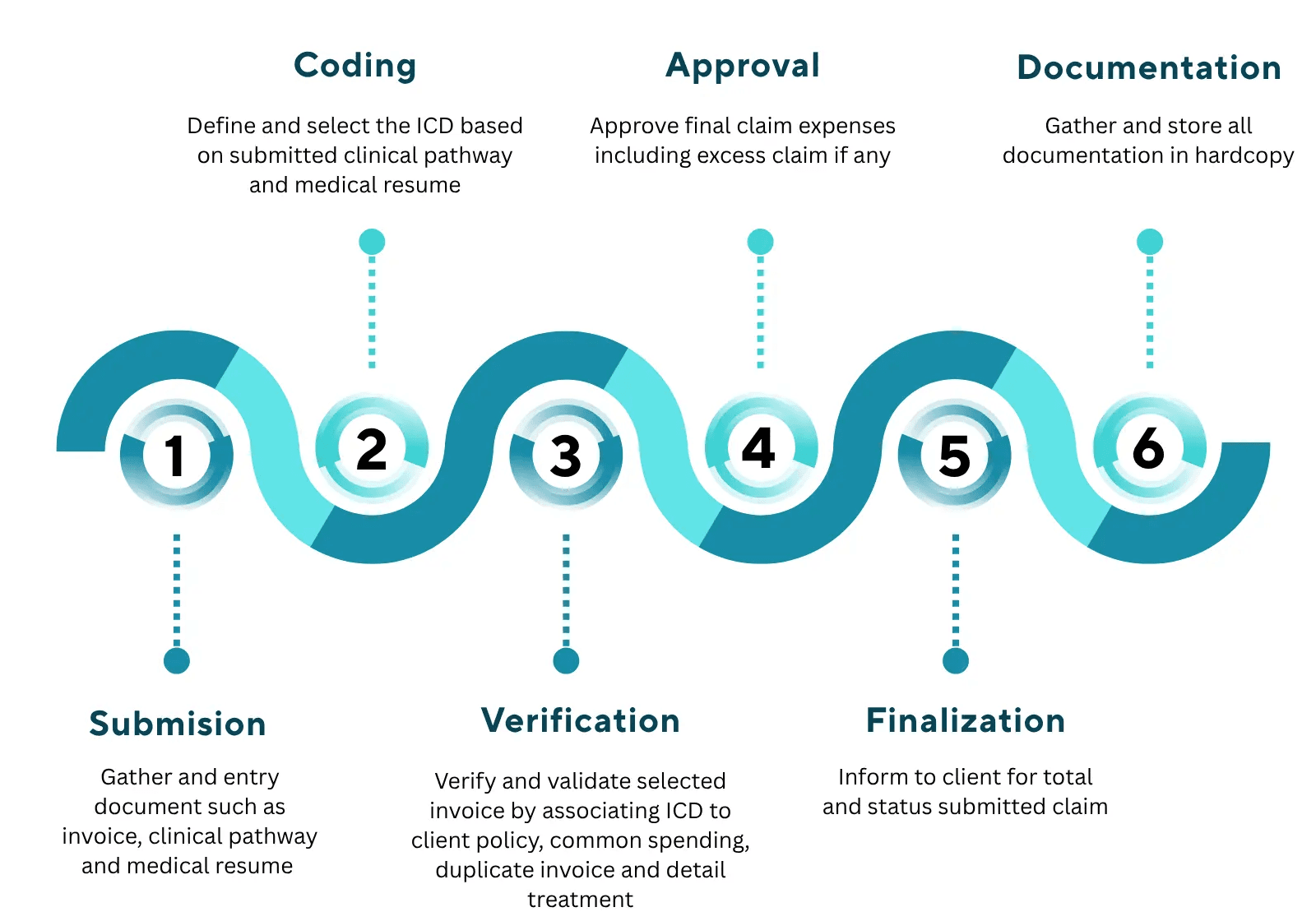
Long and manual process in insurance medical claim
It takes long waiting time for patient to settle out their claim
To stay competitive Insurers must transform how they handle risk, control costs, and run operations
The future of insurance lies in intelligence – AI doesn’t just automate tasks, it empowers insurers to predict, prevent, and perform smarter
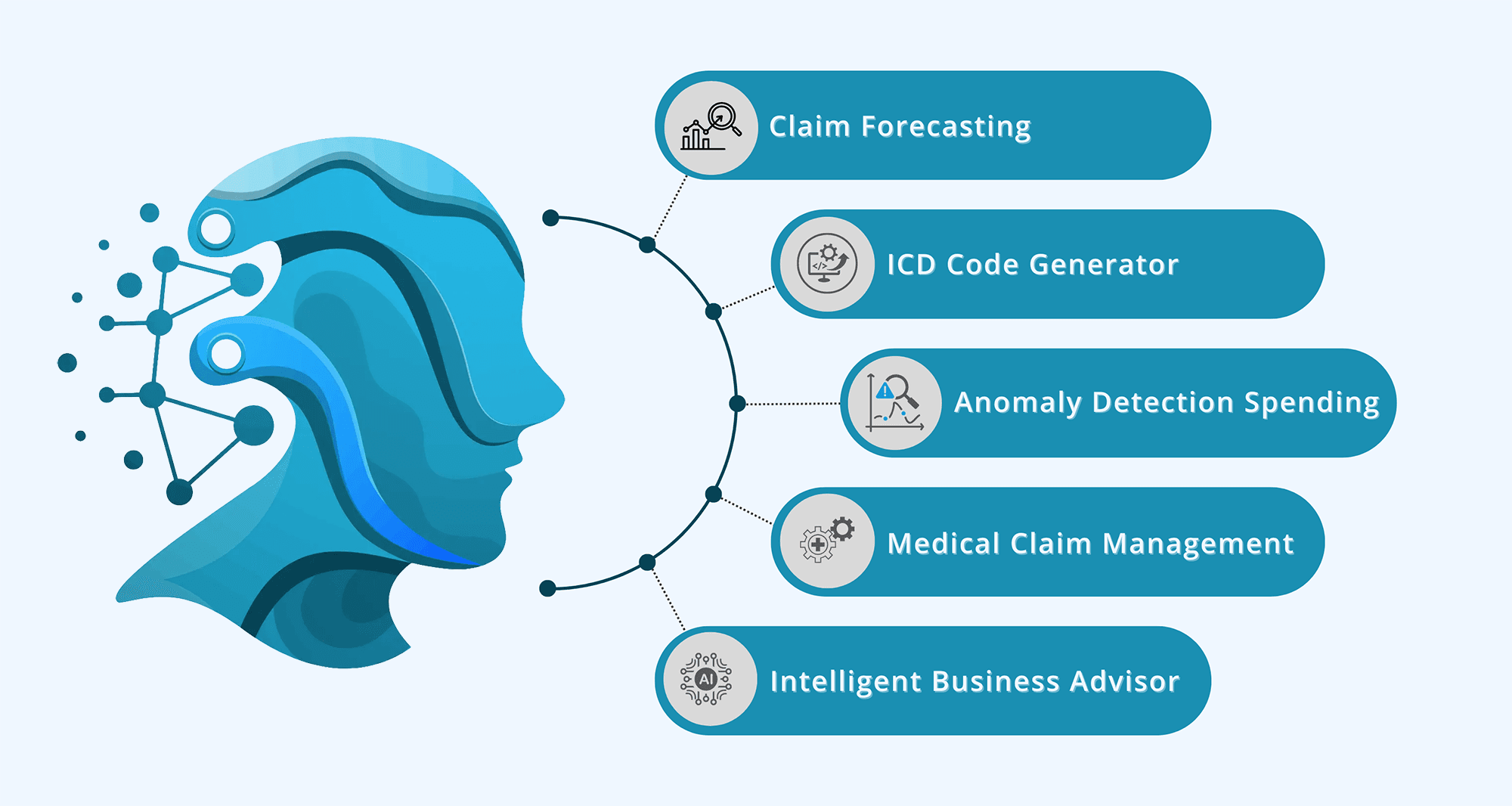
Discover Our Product
Transforming Insurance Economics with AI Claim Forecasting
Predict claim volumes and costs with precision. Our platform helps insurers optimize reserves, improve cash flow, and respond to risk in real time. Stay ahead with proactive resource planning and data-driven insights that power smarter underwriting, pricing, and product strategies.
Predict and Prepare
Accurate claim volume and cost predictions, helping you optimize reserves, improve cash flow, and eliminate wasteful over-reserving
Smarter Reserve Management
By forecasting claim surges, you can allocate resources proactively
Real-Time Risk Intelligence
Insights from claim trends feed into underwriting, pricing, and even product design — driving data-driven growth strategies
ICD Code Generators automatically and accurately assign the codes from clinical documentation
Our AI-powered ICD Code Generator automatically assigns accurate codes from clinical documentation, reducing errors, claim denials, and audits. By automating this labor-intensive task, it cuts administrative costs and scales effortlessly—handling millions of records with speed and consistency for large providers and claim administrators.
Accuracy & Compliance
Manual coding is prone to human error. AI ensures the right codes are assigned based on full clinical context, reducing claim denials & audits
Reduced Administrative Costs
Automates one of the most labour-intensive tasks in medical billing, cutting down reliance on large coding teams
Scalability, Speed & Efficiency
AI can handle millions of records with consistent performance — especially critical for large providers or claim administrators
Anomaly Detection Claim Spending automatically identify unusual or suspicious patterns in healthcare or insurance claim expenses
Our Anomaly Detection for Claim Spending uses AI to automatically identify unusual or suspicious patterns in healthcare and insurance claims. By spotting irregularities like inflated charges, duplicate claims, or atypical provider behavior early, it helps prevent fraud and financial leakage. With real-time monitoring, you can take proactive action to control costs and protect your bottom line before unnecessary expenses occur.
Detect Fraud & Abuse Early
Spot irregular claim patterns (e.g. inflated charges, duplicate submissions, unusual provider behaviour) before payouts are made
Prevent Financial Leakage
Reduce unnecessary spending by flagging outliers in procedure costs, frequency, or provider behaviour that deviate from benchmarks
Enable Real-Time Monitoring
Monitor spending in real time to take proactive action — not after the financial damage is done
Medical Claim Management is turning a complex, manual, and error-prone process into a fast, automated, and intelligent system
Our Medical Claim Management system transforms the traditionally complex and error-prone claims process into a fast, automated, and intelligent workflow. By automating data entry, validation, and approvals, it accelerates claim processing for quicker reimbursements. It also ensures accurate application of policy rules, coding standards, and compliance requirements—reducing errors, rejections, and fraud. Plus, by automating repetitive tasks like document handling and eligibility checks, it significantly lowers operational costs and administrative burdens
Faster Claim Processing
Reduce turnaround time by automating data entry, validation, and approval workflows — leading to quicker reimbursements for providers and members
Lower Operational Costs
Automate repetitive tasks (e.g., document handling, eligibility checks, rule validation), cutting down on manual labour and administrative overhead
Improved Accuracy & Compliance
Ensure correct application of policy rules, ICD/procedure codes, benefit limits, and regulatory standards — minimizing errors, rejections, and fraud
What if every business decision was powered by AI that never sleeps?
Real-time analytics powered by autonomous AI puts instant insight at your fingertips, enabling your organization to analyze and respond to changes as they happen. With our no-code platform, business users and decision-makers can ask questions in natural language and get immediate, relevant answers—no coding or data science skills needed.
Real-Time Analytics
Instant insight is no longer a luxury - it's a necessity. With autonomous AI, your organization can analyse and respond to changes as they happen
No Code
Empower business users, executives, and decision-makers to ask questions in natural language and receive immediate, relevant answers - no coding, no data science expertise require
Strategic Partners
We collaborate with industry leaders to deliver comprehensive AI solutions that drive innovation and transform business operations across various sectors.



Leadership Team
Experienced leaders combining predictive AI and generative AI to build intelligent solutions that never sleep
Get in Touch with Our Team
Whether you're looking to learn more about our solutions or explore a potential collaboration, we're ready to assist you
By clicking “Get in Touch” I agree and accept that MTA will contact me and keep me informed by sending occasional marketing communications. Read our privacy policy on how and why we might collect, store, use, and/or share your information when you use our services.

Business Office
Artha Graha Tower, 26 Floor (SCBD) Unit 2601, South Jakarta, 12190
Call Us
0877 7081 8009
Tech Hub
The Sadhana Office Space, Lavionda No.Raya 31 blok I.5, RW.7, Serpong, South Tangerang, 15321
Our Products
- Intelligent Medical Claim Agent (IMCA)


